
















When your baby cries at bedtime, it can turn what should be the most peaceful part of your day into an exhausting struggle. You're not alone—research shows that crying at bedtime affects most babies and is completely normal, especially during developmental milestones and sleep transitions.
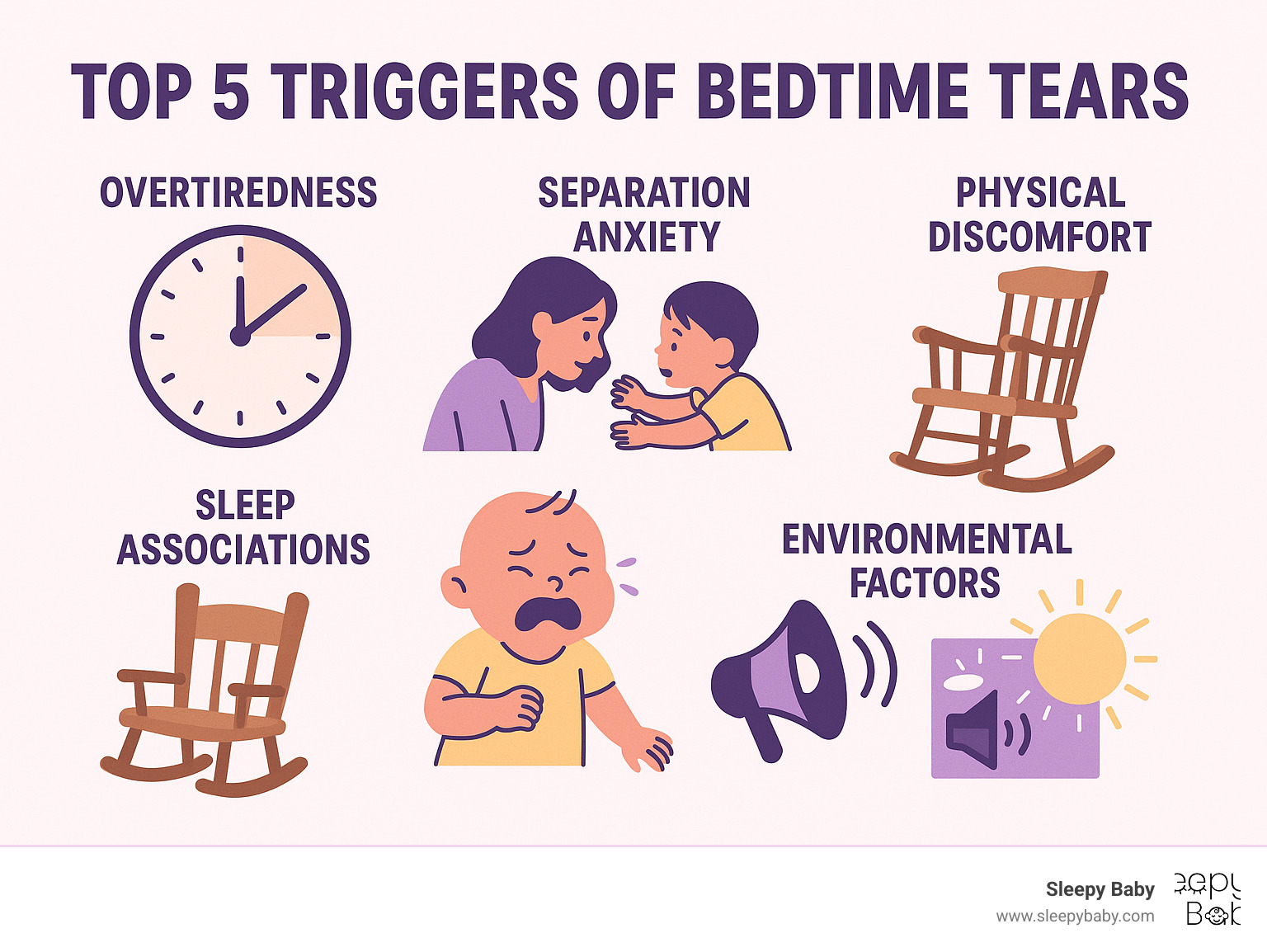
Quick Answer: Top 5 Reasons Baby Cries at Bedtime
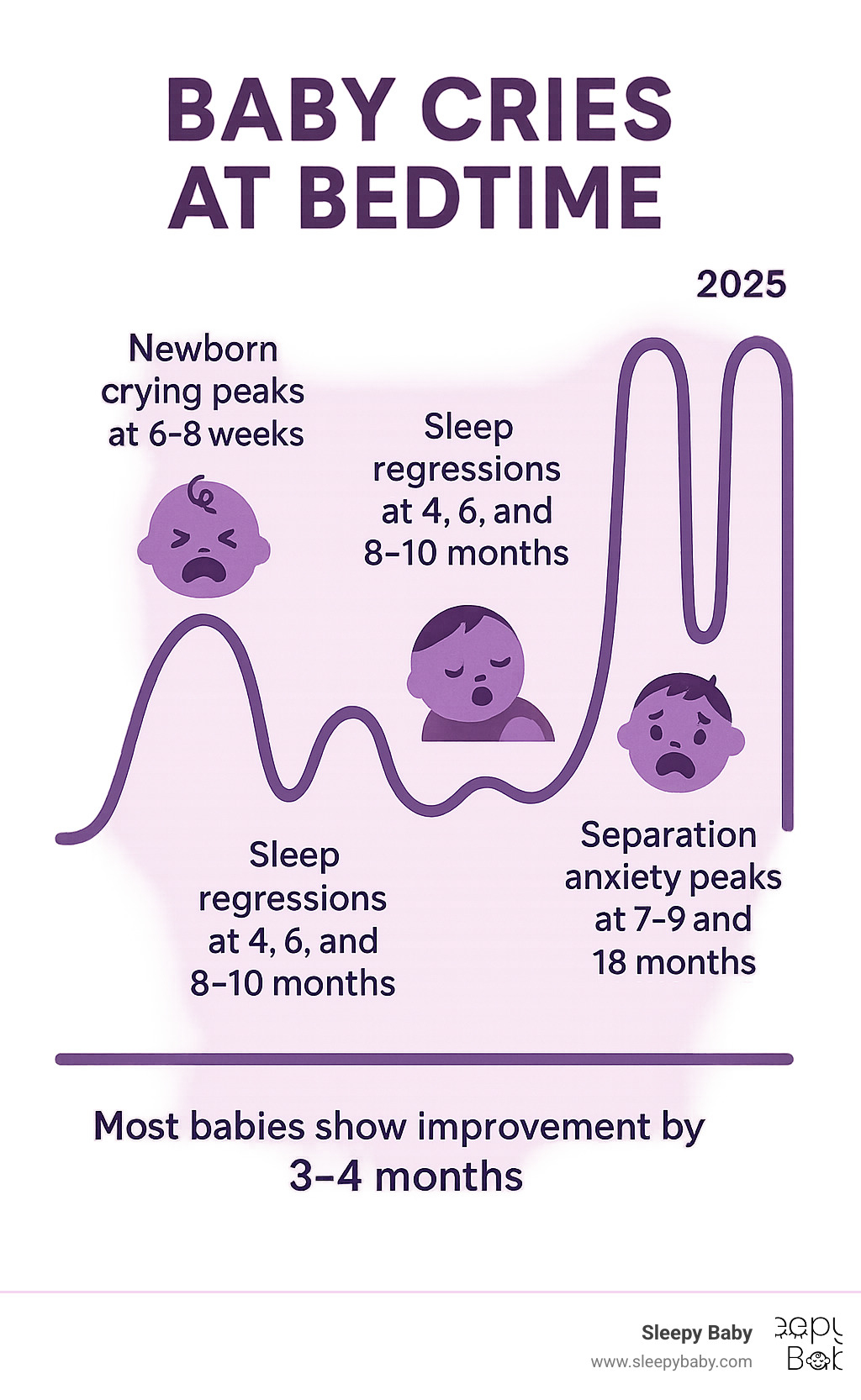
The good news? Most bedtime crying is temporary and fixable. Studies show that babies typically settle into better sleep patterns between 3-4 months as their circadian rhythms mature. Even after sleep training, some protest crying is normal—it's often your baby's way of releasing tension or asserting independence.
As Gary Harutyunyan, I understand this struggle after experiencing sleepless nights when my own newborn couldn't settle, which led me to develop solutions for families facing the same challenge of your baby cring at bedtime. My experience as both a father and someone who's helped countless families find rest has taught me that the right approach can transform bedtime from chaos to calm.
Picture this: it's 7 PM, you've dimmed the lights, started the gentle bedtime routine, and then... the crying begins. If this sounds familiar, take a deep breath. When your baby cries at bedtime, there's actually a fascinating mix of biology and development at play.
Your baby's sleep system is like a complex puzzle that's still being assembled. Unlike adults who have mature circadian rhythms, babies don't develop strong day-night cycles until around 12 weeks of age. Their internal clock is literally learning what "bedtime" means.
Healthy babies can cry 2-3 hours daily during their first months. Researchers call the peak crying period around 6-8 weeks "PURPLE crying"—and yes, bedtime often gets the worst of it.
Developmental milestones turn your baby's brain into a 24/7 construction zone. During their first year, babies form an incredible 700-1,000 fresh neural connections per second. All this brain building means sleep regressions commonly hit at 4, 6, 8-10, and 12 months.
The key is understanding protest crying versus pain crying. Protest crying usually sounds like "I don't want bedtime!"—it's your baby asserting their independence. Pain crying tends to be more intense and comes with other warning signs like fever or changes in eating.
When babies become overtired, their bodies release cortisol—the same stress hormone that keeps adults tossing and turning. This creates a cruel cycle where missing the sweet sleep window makes babies fight sleep even harder.
Absolutely, positively yes. When your baby cries at bedtime, you're witnessing your little one's brain learning one of life's most important skills: how to self-soothe. Think of it as emotional boot camp—challenging in the moment, but building strength for the future.
Crying serves as your baby's emotional release valve. Just like you might feel wound up after a busy day, babies use crying to discharge all the excitement and stimulation from being awake.
Many sleep experts actually see some bedtime crying as a positive sign. It shows your baby understands the bedtime routine and has developed enough awareness to have preferences. That's healthy independence in action.
The goal isn't to eliminate all crying immediately—that's neither realistic nor necessary. Most babies over 4 months can learn to settle within 5-15 minutes of bedtime protests.
Don't throw in the towel if your baby is still having bedtime tears after sleep training. You might be experiencing an "extinction burst"—a temporary increase in crying that happens when any established habit changes.
Consistency gaps can accidentally extend the crying phase. If you sometimes respond to bedtime protests and sometimes don't, you've created what behaviorists call "variable reinforcement"—like a slot machine that pays out randomly. This actually makes the crying stronger and last longer.
Even small routine shifts can trigger renewed tears. A different caregiver doing bedtime, traveling, or daylight saving time can all disrupt your carefully established patterns.
Habit change takes time for little brains to process. What feels like failure might actually be progress in disguise—your baby is learning, even when it doesn't sound like it.
More info about nighttime struggles
When your baby cries at bedtime, playing detective can help you solve the mystery faster than trying random solutions. Think of yourself as a sleep investigator—the clues are there, you just need to know what to look for.
Watch your little one throughout the day, not just at bedtime. Your baby's behavior during afternoon play and feeding times can reveal whether tonight's tears stem from being too tired, not tired enough, or something else entirely.
Overtired babies often seem wired rather than sleepy. They might arch their backs, become fussy during normally peaceful activities, or show that glazed, "thousand-yard stare" look.
Under-tired babies present the opposite problem—they seem genuinely ready to party at 7 PM. They're alert, playful, and might even smile at you from their crib.
Separation anxiety has its own signature. The crying often changes when you enter or leave the room, and you might notice your baby reaching toward you or the door.
Physical discomfort shows up in specific ways. Babies with gas might draw their legs up to their bellies. Reflux often causes crying that worsens when lying flat. Teething pain can make babies want to chew on everything during the day and cry more at night.
Here's a quick comparison to help you decode what you're seeing:
| Sleepy Cues | Distress Signs |
|---|---|
| Yawning, eye rubbing | Arching back, rigid body |
| Slower movements | Frantic movements |
| Quieter vocalizations | High-pitched, urgent crying |
| Seeking comfort | Pushing away comfort |
| Droopy eyelids | Wide, alert eyes |
Environmental factors are the sneaky culprits parents often miss. Even a sliver of light from a hallway, the neighbor's dog barking, or a room that's too warm can trigger sensitive babies to cry.
Getting wake windows right feels like hitting a moving target, but it's one of the most important pieces of the bedtime puzzle. Think of it as your baby's internal timer—miss the sweet spot, and you're in for a rough night.
Wake window math changes constantly as babies grow. A 1-month-old can typically handle about one hour of awake time, while a 3-month-old might manage up to two hours. Missing these windows by even 15-30 minutes can be the difference between peaceful sleep and a crying marathon.
When babies become overtired, their bodies flood with cortisol—the same stress hormone that keeps adults awake after a difficult day. This creates a cruel irony: the more exhausted your baby becomes, the harder it is for them to actually fall asleep.
Late afternoon naps are frequent troublemakers. If your baby snoozes past 3 or 4 PM, they might not build up enough "sleep pressure" for bedtime.
Chronic overtiredness builds up over days or weeks. If your baby has been consistently under-sleeping, you might need a "reset day" with earlier bedtimes and longer naps to break the cycle.
Around 6-7 months, your baby's brain makes an incredible leap—they develop object permanence, which means they finally understand that you exist even when they can't see you. While this is amazing for development, it can turn bedtime into a tearfest.
The crying during separation anxiety sounds different from other bedtime protests. It's often more urgent and desperate, and you might hear your baby calling out or see them reaching toward the door. Unlike other types of crying, it usually gets worse when you appear and then leave again.

The 18-month regression brings a second wave of separation anxiety as toddlers become more aware of their independence while still craving security.
The key is offering reassurance without accidentally creating new problems. Brief, boring check-ins can help your baby feel secure without teaching them that crying brings extended playtime with mom or dad.
Sometimes when your baby cries at bedtime, their body is trying to tell you something important. Physical discomfort is surprisingly common but often gets overlooked when parents assume all bedtime crying is behavioral.
Reflux can be a sneaky culprit because lying flat makes stomach acid more likely to creep up. Your baby might seem fine during the day but struggle once horizontal.
Teething pain often intensifies at night when there are fewer distractions. During the day, toys and activities help babies forget about sore gums, but bedtime brings focus back to the discomfort.
Ear infections are notorious bedtime disruptors because lying flat increases pressure and pain. If crying seems to worsen when your baby is horizontal, especially with fever or ear-pulling, it's time to call the pediatrician.
Temperature guidelines for seeking medical care: under 2 months, any fever of 100.4°F or higher needs immediate attention. For 3-6 months, call for fevers over 101°F. Six months and older can usually wait unless fever reaches 103°F or is accompanied by other concerning symptoms.
Trust your instincts—you know your baby better than anyone. If something feels wrong beyond normal bedtime fussiness, don't hesitate to seek professional guidance.
Scientific research on safe sleep
When your baby cries at bedtime, you need practical solutions that actually work. These evidence-based strategies have helped thousands of families transform bedtime battles into peaceful wind-downs.
Think of your bedtime routine as your baby's daily preview of what's coming next. Research shows that babies who have consistent routines cry less and fall asleep faster because their brains learn to anticipate sleep.
Your routine should flow like a gentle river—each step naturally leading to the next. Start with bath time or a gentle wash, then move to feeding (but finish this 15-20 minutes before putting baby down). Follow with quiet activities like reading a short book or singing soft songs. End with your final goodnight using the same key phrase every night.
Keep the whole routine between 15-30 minutes. Any longer and you might actually increase your baby's anticipation and anxiety. As you move through each step, gradually dim the lights to help your baby's natural melatonin production kick in.
Avoid tickling, exciting games, or anything that gets your baby's heart racing within two hours of bedtime. Even happy excitement can make it harder for little ones to settle down.
Getting your timing right can be the difference between easy bedtime and hours of crying. Age-appropriate wake windows are your secret weapon—newborns can only handle 45 minutes to 2 hours awake, while babies 3-6 months can manage 1.5 to 3 hours, 6-9 months can stay up 2.5 to 4 hours, and 9-12 months can handle 3 to 5 hours.
Your baby's individual cues matter more than any chart. Watch for early sleepy signals like yawning, eye rubbing, or getting quieter. These are your green lights to start the bedtime routine, even if the clock says it's "too early."
If you've missed that sweet spot and your baby is overtired, don't panic. Sometimes moving bedtime earlier—even as early as 5:30 PM—can help reset an overtired baby's system and reduce crying.
Your baby's sleep environment can make or break bedtime success. The goal is creating a space that whispers "sleep time" to your baby's developing brain.
Darkness is your friend. Use blackout curtains or coverings because even tiny amounts of light can interfere with your baby's natural sleep hormones. Keep the room cool but comfortable—between 68-72°F works best.
White noise can be magical for settling fussy babies. It masks household sounds and provides consistent audio cues that signal sleep time. Just keep the volume at or below 50 decibels—about as loud as a quiet conversation.
Finally, make the room visually calm. That adorable mobile might be perfect for playtime, but it can be distracting when your baby should be settling down.

When baby cries at bedtime because they don't want you to leave, your confidence and consistency make all the difference. Separation anxiety is tough, but it's also a sign your baby is developing normally.
Create a predictable goodbye routine using the same phrase every night: "Goodnight, I love you, see you in the morning." Keep it brief and resist the urge to come back for "just one more kiss."
Around 6 months, introduce a comfort object—a small lovey or soft toy that smells like you. This gives your baby something soothing to hold onto when you're not there.
During the day, practice brief separations through games like peek-a-boo or stepping into another room for a moment before returning cheerfully.
If you need to check on your baby, keep visits brief and boring. A quick "It's sleep time" without picking up or extended interaction usually works best.
The art of soothing is about calming your baby's nervous system without creating habits that require your constant presence. It's a delicate balance, but totally achievable.
For babies under 2 months, swaddling can work wonders by controlling the startle reflex that often wakes newborns. Stop swaddling once your baby shows signs of rolling for safety reasons.
Rhythmic patting can be incredibly effective because it mimics the familiar heartbeat sounds from the womb. This is where consistent, gentle rhythmic motion really shines—providing that comforting touch that helps babies learn to self-soothe. The Sleepy Baby portable soother offers exactly this kind of hands-free, rhythmic comfort that many families find invaluable.
If you've been rocking or holding your baby to sleep, try gradually reducing the intensity. Start with less movement, then less time, then eventually just placing your hand on their chest before transitioning to independent sleep.
Keep your lullabies or white noise consistent. Many parents find success with the same gentle sounds on repeat each night, creating a reliable audio cue for sleep.
Here's a helpful way to think about consistency: imagine a vending machine that sometimes gives you a snack when you put money in and sometimes doesn't. You'd keep trying different amounts or pressing buttons harder, right? That's exactly what happens when our responses to bedtime crying are inconsistent.
Variable responses—sometimes picking up your baby, sometimes not—actually increase crying over time. Your baby learns that if they cry long enough or hard enough, the response might change.
Keep a simple journal tracking your baby's bedtime routine, how long they cried, and how you responded. This helps you spot patterns and maintain consistency.
Some crying during the learning phase is completely normal and not harmful. Research shows that teaching babies to self-settle doesn't damage your bond when done with love and consistency.
As a parent, you know your baby better than anyone. While most bedtime crying is completely normal, there are times when your instincts might tell you something isn't quite right. Trust those feelings—they're usually spot-on.
Some crying patterns require immediate attention. If your baby cries at bedtime and the sound seems different—more urgent, high-pitched, or desperate than usual—it's worth investigating further. Babies under two months with any fever (100.4°F or higher) need medical attention right away.
Watch for signs that crying might indicate illness rather than typical bedtime resistance. Vomiting, diarrhea, or a rash combined with fever are red flags. If your baby seems to be in genuine pain when lying flat, this could signal reflux, an ear infection, or other medical issues.
Changes in your baby's normal patterns can also signal trouble. Fewer wet diapers than usual, significant changes in eating habits, or weight loss alongside persistent crying warrant a call to your pediatrician.
Colic presents its own challenges—affecting up to 20% of babies with crying sessions lasting more than three hours daily, at least three days per week. While incredibly stressful for families, colic typically resolves by three to four months.
Sometimes the issue isn't your baby—it's you, and that's completely okay. Parental burnout from sleep deprivation is real and serious. When you're exhausted, your ability to think clearly and care for your baby safely can be compromised.
If you've been consistent with your bedtime routine for two weeks without improvement, or if you're feeling overwhelmed, anxious, or depressed, it's time to reach out for support.
You don't have to steer this alone. Multiple types of professionals can offer support when your baby crying at bedtime becomes overwhelming.
Your pediatrician should be your first call for any health concerns. Many pediatric offices have nurse hotlines available for after-hours questions—don't hesitate to use them.
Certified sleep consultants can provide personalized strategies custom to your family's unique situation and parenting style. They can help identify specific issues you might be missing and create a step-by-step plan that works for your household.
If you're struggling with your own mental health, specialized perinatal mental health services are available in most areas. Postpartum depression and anxiety are incredibly common—you're not alone, and effective help is available.
Lactation consultants can be lifesavers if breastfeeding challenges are contributing to bedtime struggles. Sometimes feeding issues create a domino effect that impacts sleep.
Consider scheduling a complimentary consultation to discuss your specific situation with a sleep specialist who can provide personalized guidance.

Seeking help isn't admitting failure—it's being the best parent you can be. Every baby is different, and what works beautifully for your neighbor's child might not work for yours.
Most bedtime crying phases are temporary, lasting anywhere from a few days to a few weeks. For newborns experiencing normal developmental crying, expect improvement around 3-4 months as circadian rhythms mature. Sleep regressions typically last 2-6 weeks.
If you're implementing new sleep strategies, give them at least 1-2 weeks of consistency before expecting significant change. Some babies adapt quickly, while others need more time to learn new skills.
Protest crying usually:
Pain crying typically:
When in doubt, always check for physical causes first—hunger, dirty diaper, temperature, or signs of illness.
Yes, sudden routine changes can temporarily increase crying. Babies thrive on predictability, and even positive changes can be disruptive initially.
If you need to modify your routine, make changes gradually when possible. For example, if you want to move bedtime earlier, shift it by 15 minutes every few days rather than making a dramatic change all at once.
However, some changes are necessary and worth the temporary disruption. If your current routine isn't working, the short-term increase in crying often leads to better long-term sleep.
When your baby cries at bedtime, you're witnessing your little one's journey toward independence—not a sign of your parenting skills. Those tears at bedtime are actually your baby's way of learning one of life's most important skills: how to soothe themselves to sleep.
Think of this phase as temporary growing pains. Just like learning to walk involves some tumbles, learning to sleep independently involves some protest. Most families see significant improvement within 2-4 weeks of consistent effort, and the investment pays dividends for years to come.
Your path forward starts with identifying what's driving the tears—whether it's overtiredness, separation anxiety, or environmental factors. Once you know the "why," you can choose the right strategy from our toolkit. Remember to implement one change at a time rather than overwhelming yourself and your baby with multiple new approaches.
Give your chosen strategy time to work. It's tempting to switch tactics after a rough night or two, but consistency is your secret weapon. Most sleep changes need at least 1-2 weeks to take hold, especially if you're helping your baby unlearn old habits.
Consider keeping a simple journal—even notes on your phone work. Track bedtime, how long crying lasts, and what you tried. You'll start seeing patterns that guide your next steps.
Celebrate the small victories along the way. If crying drops from 45 minutes to 20 minutes, that's real progress worth acknowledging. If your baby settles faster after their bedtime routine, you're building positive associations.
Every baby writes their own sleep story. Your neighbor's baby who slept through the night at 8 weeks isn't the standard—they're just one example. Your baby might need more time, different strategies, or a gentler approach. Trust your instincts about what feels right for your family.
Don't hesitate to build your support network during this challenging time. Whether that's connecting with other parents online, calling a friend who's been through this, or consulting with a sleep professional, you don't have to figure this out alone.
The sleepless nights and bedtime tears you're experiencing now won't last forever. With patience, consistency, and the right approach for your unique baby, you'll help them develop healthy sleep habits that benefit your entire family. Those peaceful bedtimes and full nights of sleep are closer than they seem.
More info about self-soothing techniques
Sweet dreams are coming—for both you and your little one.